This designation indicates the physical location where a healthcare professional renders services to a patient. Specifically, it signifies an office setting, typically a physician’s office, where patients receive medical evaluations, treatments, or consultations. This location is characterized by its primary function as a dedicated space for outpatient healthcare delivery. As an example, a patient visiting a cardiologist for a routine check-up in their private practice would have services rendered under this classification.
Its significance lies in its use for proper claims processing and reimbursement within the healthcare system. It enables accurate tracking of healthcare utilization patterns and facilitates data analysis for quality improvement initiatives. Historically, the establishment of standardized location codes like this aimed to bring clarity and uniformity to the complex landscape of healthcare billing. This standardization has improved efficiency in administrative processes and fostered greater transparency in healthcare finance.
Understanding location coding is crucial for healthcare providers, billing specialists, and anyone involved in healthcare administration. Accurate reporting ensures appropriate payment for services rendered and contributes to the overall integrity of the healthcare system. The following sections will delve into related topics, exploring variations in location coding, the impact on reimbursement rates, and best practices for accurate documentation.
1. Physician office setting
The physician office setting is intrinsically linked to place of service code 11. This code explicitly denotes that the healthcare service was rendered within the confines of a doctor’s office or similar outpatient facility. The relationship is one of direct correspondence; the physical location (physician’s office) is the determining factor for applying the specific code. For instance, if a patient receives an annual physical examination at their primary care physicians office, the claim submitted to the insurance company would include this designation. The causal relationship is clear: the service occurs in a physician’s office; therefore, this designator is appropriate.
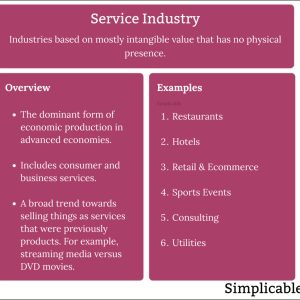
Suggested read: Comprehensive Guide to the Service Industry Definition
The importance of accurately identifying a physician office setting is paramount for proper claim adjudication. Incorrectly coding a service performed in this location, such as using a code for a hospital outpatient department, can lead to claim denials or payment errors. Consider a scenario where a minor surgical procedure is performed in a physician’s office equipped for such interventions; using a different code could imply the use of more extensive facilities and result in incorrect reimbursement. Real-world examples frequently highlight the administrative burdens and financial losses associated with inaccurate coding practices. Moreover, the data collected using these codes inform healthcare policy decisions and resource allocation strategies.
In summary, the connection between a physician office setting and this location code is fundamental to the accurate and efficient operation of the healthcare billing system. Proper documentation and understanding of coding guidelines are essential to avoid claim errors and ensure appropriate reimbursement. Addressing challenges in coding accuracy requires ongoing education and training for healthcare providers and billing staff. This detailed approach supports the broader goals of maintaining transparency and accountability within the healthcare finance framework.
2. Outpatient service location
The designation directly correlates with outpatient service locations. As a standardized code, it precisely defines a healthcare setting where medical services are provided to patients who do not require overnight hospitalization. Its selection indicates that the services were rendered in a facility designed for ambulatory care, such as a private practice, clinic, or similar setting. The causal relationship is that outpatient treatment is the defining characteristic of the location requiring the application of this code; without outpatient care being delivered, the code would be inappropriate. For example, a patient receiving a routine vaccination at their family doctor’s office would have services coded accordingly, reflecting the outpatient nature of the visit.
The significance of accurately identifying the outpatient service location through this code is paramount for correct claims processing and reimbursement. Incorrectly classifying a service as occurring in an inpatient setting, or vice versa, can lead to claim denials, reduced payments, or even audits. A tangible illustration can be seen in a scenario where a patient receives physical therapy at an outpatient rehabilitation center; miscoding this service could result in significant financial repercussions for the provider. Furthermore, these location codes are used for data analysis to understand healthcare utilization patterns. For instance, public health officials might track the number of vaccinations administered in outpatient settings to monitor immunization rates and plan public health campaigns.
In summation, the association between outpatient service locations and this location code is critical to the integrity of the healthcare billing system. The practical significance lies in ensuring accurate reimbursement, promoting data-driven decision-making, and supporting the overall financial health of healthcare providers. Addressing challenges such as ambiguous service definitions and the need for ongoing training is essential to maintain accuracy and compliance within this system. The continued evolution and refinement of coding guidelines are vital to reflecting the changing landscape of outpatient healthcare delivery.
3. Billing code accuracy
Billing code accuracy is inextricably linked to place of service 11. The accuracy of billing codes, including the precise identification of the service rendered and its corresponding location code, directly impacts reimbursement rates and claim processing. When place of service 11, denoting a physician’s office, is accurately applied in conjunction with appropriate CPT or HCPCS codes, it signals to payers the specific setting in which the medical service was provided. This, in turn, determines the applicable fee schedule and payment amount. A causal relationship exists wherein inaccurate coding leads to claim denials, delays in payment, or even audits, while precise coding facilitates smooth and timely reimbursement. A real-life example would be a claim for an injection administered in a physician’s office; the correct use of place of service 11, paired with the appropriate injection code, ensures proper payment according to the office-based fee schedule.
The accurate application of billing codes with place of service 11 extends beyond individual claims. Aggregated data derived from these codes provides valuable insights into healthcare utilization patterns and costs. This data is utilized by healthcare administrators, researchers, and policymakers to inform resource allocation, develop clinical guidelines, and evaluate the effectiveness of healthcare programs. Furthermore, accurate billing practices contribute to the integrity of healthcare data, ensuring that statistical analyses and reports are based on reliable information. Consider the scenario of tracking the prevalence of influenza vaccinations in a community; accurate place of service coding, including the identification of vaccinations administered in physicians’ offices, is crucial for generating reliable statistics and informing public health interventions.
In summary, billing code accuracy is a critical component of place of service 11. It directly influences reimbursement, facilitates data-driven decision-making, and supports the integrity of healthcare information. Challenges in maintaining accuracy stem from the complexity of coding guidelines, the need for ongoing training, and the potential for human error. Addressing these challenges requires a multi-faceted approach, including implementing robust coding protocols, providing continuous education for billing staff, and leveraging technology to automate coding processes and reduce errors. The consistent application of accurate billing codes contributes to a more efficient and transparent healthcare system.
4. Reimbursement rates impact
The determination of reimbursement rates is significantly affected by the designated place of service, with location code 11 (physician’s office) serving as a pivotal factor. Understanding this impact is crucial for healthcare providers, as it directly influences revenue cycles and financial planning.
-
Standard Fee Schedules
Payers, including both government entities and private insurance companies, establish standard fee schedules that vary based on the location where services are rendered. Physician’s office settings often have different reimbursement rates compared to hospital outpatient departments or ambulatory surgical centers. This differentiation reflects the cost structure and overhead associated with each type of facility. For example, a standard office visit coded with location code 11 will typically be reimbursed at a rate specific to that setting, which may be lower than the rate for the same service performed in a hospital.
Suggested read: Instant, Accurate Service Quotes - Get Your Project Started Today!
-
Contract Negotiations
The place of service code influences contract negotiations between healthcare providers and insurance companies. Providers may negotiate higher reimbursement rates for services performed in their offices based on factors such as the complexity of the services offered, the cost of maintaining the facility, and the patient population served. A physician group specializing in complex cardiology services, for instance, might negotiate higher rates for office-based procedures, citing the specialized equipment and highly trained staff required to deliver that care.
-
Bundled Payments
The assignment of location code 11 is critical in the context of bundled payment arrangements. These arrangements involve a single payment for all services related to a specific episode of care. Accurately identifying the place of service helps determine which services are included in the bundle and the overall reimbursement amount. If a patient undergoes a series of office visits, diagnostic tests, and follow-up care within a physician’s office as part of a bundled payment arrangement, the correct coding of these services with this location code is essential for proper payment reconciliation.
-
Compliance and Audits
The accurate assignment of location codes is essential for compliance with billing regulations and to avoid potential audits. Misrepresenting the place of service can lead to overpayment or underpayment and may trigger scrutiny from payers. For example, if a provider inappropriately codes a service performed in a physician’s office as being performed in a hospital setting to receive a higher reimbursement, this could be considered fraudulent billing and result in significant penalties.
In conclusion, location code 11 plays a significant role in determining reimbursement rates for services rendered in physician’s offices. Understanding the impact of this code is essential for healthcare providers to ensure accurate billing, negotiate favorable contracts, and maintain compliance with billing regulations. The complexities associated with reimbursement underscore the need for ongoing education and training for billing staff and healthcare professionals.
5. Data analysis relevance
Location code 11, denoting services rendered in a physician’s office, is a critical element in healthcare data analysis. Its impact stems from its ability to categorize and differentiate healthcare utilization patterns. The code allows for specific extraction and analysis of data related to services provided within this particular outpatient setting. The causal relationship is such that the presence of location code 11 within claims data enables researchers and healthcare administrators to isolate and examine trends, costs, and outcomes specifically associated with physician office visits. For instance, a study examining the effectiveness of a new medication may focus on data points derived solely from claims bearing this code to accurately assess its impact within a standard outpatient environment. The codes reliability is thus directly proportional to the data’s analytical value.
The importance of location code 11 for data analysis lies in its ability to provide granularity. Without this level of specificity, it would be challenging to differentiate between services delivered in different settings, leading to less precise and potentially misleading insights. For example, analysis of preventive care services, such as vaccinations or screenings, can be significantly enhanced by isolating data from physician offices. This enables a more accurate understanding of access, delivery, and effectiveness within a routine clinical environment. A practical application is the tracking of chronic disease management in outpatient settings, facilitating improvements in care coordination and patient outcomes. This precise setting identification contributes significantly to resource allocation and informs policy decisions aimed at enhancing primary care access.
In summary, the application of location code 11 holds substantial relevance for healthcare data analysis. Its accurate and consistent utilization enhances the precision and reliability of derived insights, which in turn support informed decision-making and continuous quality improvement initiatives. Addressing challenges related to coding accuracy and data integrity is essential to maximize the potential benefits. The proper application and interpretation of data linked to location code 11 contribute significantly to a more efficient and effective healthcare system.
Frequently Asked Questions Regarding Place of Service 11
This section addresses common inquiries related to the utilization and implications of location code 11 within the healthcare billing system.
Suggested read: User-Friendly Service Project Ideas for the Service-Minded
Question 1: What constitutes a valid setting for the application of location code 11?
Location code 11 is appropriately used when healthcare services are rendered within a physician’s office. This encompasses private practices, group practices, and other outpatient settings where a physician provides medical care.
Question 2: How does the designation impact reimbursement rates?
The designation influences reimbursement as payers establish fee schedules based on the place of service. Physician office settings typically have different reimbursement rates than hospital outpatient departments. Accurate coding ensures appropriate payment.
Question 3: What are the potential consequences of inaccurate coding with location code 11?
Inaccurate coding can lead to claim denials, delays in payment, or audits by payers. Misrepresenting the place of service to obtain higher reimbursement is considered fraudulent and may result in penalties.
Question 4: How is it utilized in healthcare data analysis?
The code enables researchers and healthcare administrators to analyze data related to services specifically provided in physician offices. This facilitates understanding healthcare utilization patterns, cost trends, and outcomes within that setting.
Question 5: Is specific documentation required to support the use of it?
Yes, documentation must clearly support that the services were rendered in a physician’s office. This includes patient records, encounter forms, and other relevant documentation that accurately reflect the place of service.
Suggested read: Ultimate Guide to Service Marks: Protecting Your Brand Identity
Question 6: What are common mistakes to avoid when applying it?
Common mistakes include confusing a physician’s office with a hospital outpatient department or an urgent care center. Careful attention to the specific location where services are rendered is crucial for accurate coding.
In summary, a thorough understanding of the appropriate application and implications of location code 11 is essential for accurate billing, compliant practices, and effective healthcare data analysis.
The following section will explore best practices for ensuring accurate documentation and coding related to place of service 11.
Tips for Accurate Place of Service 11 Coding
The following guidelines are designed to assist healthcare providers and billing staff in ensuring accurate application of location code 11, representing services rendered in a physician’s office.
Tip 1: Verify the Physical Location. Prior to assigning location code 11, confirm that the service was indeed provided within the confines of a physician’s office or a similar outpatient facility dedicated to physician services. Misidentification of the location can lead to claim denials.
Tip 2: Distinguish from Similar Settings. Differentiate the physician’s office from hospital outpatient departments, urgent care centers, and other ambulatory care settings. The key distinction is the primary role of a licensed physician in providing care within the office setting.
Tip 3: Utilize Comprehensive Documentation. Maintain thorough and accurate documentation that clearly indicates the place of service. This includes patient records, encounter forms, and billing records that corroborate the assignment of location code 11.
Tip 4: Stay Updated on Coding Guidelines. Regularly review updates and revisions to coding guidelines and payer policies related to place of service coding. Changes may occur periodically, impacting proper application of location code 11.
Tip 5: Conduct Regular Audits. Implement a process for periodic internal audits of billing practices to identify and correct any coding errors related to place of service. This helps ensure ongoing accuracy and compliance.
Tip 6: Provide Staff Training. Ensure that all billing and coding staff receive comprehensive training on place of service coding, including specific guidance on when and how to apply it. Ongoing education is essential for maintaining accuracy.
Suggested read: The Essential Guide to Finding a Top-Notch Service Professor
Tip 7: Leverage Technology. Utilize electronic health record (EHR) systems and billing software to automate coding processes and reduce the risk of human error. These tools can assist in identifying and preventing inaccurate place of service coding.
Adhering to these tips promotes accurate coding, reduces claim denials, and supports compliance with billing regulations. Consistent application of these guidelines enhances the integrity of healthcare data and contributes to efficient revenue cycle management.
The subsequent section will provide a concise summary of the key principles discussed throughout this article.
Conclusion
This exploration has underscored the importance of accurate designation as a cornerstone of the healthcare billing process. The specific coding signifies services rendered within a physician’s office, impacting reimbursement, data analysis, and regulatory compliance. Adherence to established guidelines and meticulous documentation are essential for navigating the complexities of healthcare finance. The ramifications of incorrect coding can extend beyond immediate financial implications, affecting the integrity of healthcare data and potentially triggering audits.
Given its continued relevance in a constantly evolving healthcare landscape, a commitment to precision in applying location coding is paramount. Healthcare providers and billing professionals must remain vigilant in their understanding of current regulations and best practices. Continued education and rigorous internal auditing procedures represent critical safeguards. The pursuit of accuracy in coding contributes to the broader goal of a transparent and efficient healthcare system.