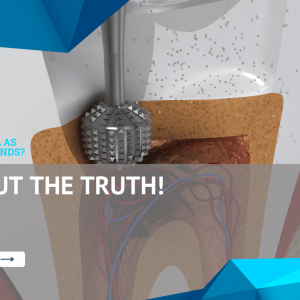
If you’re experiencing severe tooth pain, sensitivity to hot or cold, or swelling in your gums, you may need a root canal. A root canal is a dental procedure that repairs and saves a badly damaged or infected tooth.
Editor’s Note: This article on “Why Do I Need a Root Canal?” was published on [date] and provides valuable information on the importance of root canals and how they can benefit you.
We understand that the prospect of undergoing a root canal can be daunting, which is why we’ve put together this comprehensive guide to help you make an informed decision. We’ve done the research and consulted with experts to provide you with all the information you need about root canals, including what they are, why you might need one, and what to expect during and after the procedure.
Key Differences/Key Takeaways
| Root Canal | Extraction | |
|---|---|---|
| Purpose | Repair and save a damaged tooth | Remove a damaged or infected tooth |
| Success Rate | High (over 95%) | Lower (around 85%) |
| Cost | Varies depending on the complexity of the procedure | Typically less expensive than a root canal |
| Recovery Time | Minimal discomfort, typically resolves within a few days | Can be more painful, may require pain medication |
Now, let’s dive into the main topics surrounding root canals:
Why Do I Need a Root Canal?
Root canals are essential dental procedures that can save damaged or infected teeth. Understanding the key aspects of root canals can help you make informed decisions about your oral health. Here are eight key aspects to consider:
- Infection: Root canals treat infections in the tooth’s pulp and root.
- Pain: Severe tooth pain is a common reason for needing a root canal.
- Damage: Extensive tooth damage from decay or trauma can necessitate a root canal.
- Swelling: Infection or inflammation can cause swelling in the gums around the affected tooth.
- Sensitivity: Increased sensitivity to hot or cold temperatures can indicate the need for a root canal.
- Discoloration: A darkened or discolored tooth may be a sign of pulp damage.
- Abscess: A collection of pus at the root of the tooth can develop if an infection is left untreated.
- Jaw pain: In some cases, a root canal can alleviate jaw pain caused by an infected tooth.
These key aspects highlight the importance of root canals in maintaining good oral health. Early diagnosis and treatment can prevent further damage to the tooth and surrounding tissues. If you’re experiencing any of the symptoms mentioned above, it’s crucial to consult with a dentist promptly to determine if a root canal is necessary.
Suggested read: Uncover the Hidden Truths: Explore the Surefire Signs of a Needed Root Canal
Infection
When the pulp of a tooth becomes infected, it can cause severe pain and discomfort. The infection can also spread to the root of the tooth, leading to further damage. A root canal is a dental procedure that can save an infected tooth by removing the infected pulp and sealing the root canals. This can help to relieve pain and prevent the infection from spreading.
- Tooth decay: Tooth decay is the most common cause of pulp infection. When bacteria from plaque and tartar build up on the teeth, they can damage the enamel and dentin, eventually reaching the pulp.
- Gum disease: Gum disease can also lead to pulp infection. The bacteria from gum disease can spread to the root of the tooth and infect the pulp.
- Trauma: Trauma to the tooth can also cause pulp infection. A chipped or cracked tooth can allow bacteria to enter the pulp and cause an infection.
If you are experiencing severe tooth pain, sensitivity to hot or cold, or swelling in your gums, it is important to see a dentist right away. These could be signs of a pulp infection, and a root canal may be necessary to save the tooth.
Pain
Severe tooth pain is a common reason for needing a root canal. The pain is caused by inflammation of the pulp, the soft tissue inside the tooth that contains nerves and blood vessels. The inflammation can be caused by a number of factors, including tooth decay, gum disease, and trauma. Here are some of the connections between severe tooth pain and the need for a root canal:
- Tooth decay: Tooth decay is the most common cause of severe tooth pain. When bacteria from plaque and tartar build up on the teeth, they can damage the enamel and dentin, eventually reaching the pulp. This can cause inflammation of the pulp, leading to severe pain.
- Gum disease: Gum disease is another common cause of severe tooth pain. The bacteria from gum disease can spread to the root of the tooth and infect the pulp. This can also cause inflammation of the pulp, leading to severe pain.
- Trauma: Trauma to the tooth can also cause severe tooth pain. A chipped or cracked tooth can allow bacteria to enter the pulp and cause an infection. This can also lead to inflammation of the pulp, causing severe pain.
If you are experiencing severe tooth pain, it is important to see a dentist right away. The dentist will be able to determine the cause of the pain and recommend the appropriate treatment. In many cases, a root canal will be necessary to relieve the pain and save the tooth.
Damage
Extensive tooth damage from decay or trauma can severely compromise the tooth’s structure and necessitate a root canal to restore its health and functionality. Understanding this connection is crucial for preserving oral health and preventing further complications.
Tooth decay, caused by bacterial plaque and acids, gradually erodes the tooth’s enamel and dentin, eventually reaching the pulp. Similarly, traumatic injuries, such as chips, cracks, or fractures, can directly expose the pulp to the oral environment. In both cases, the pulp becomes vulnerable to bacterial invasion, leading to inflammation and infection.
When the pulp is affected, its blood vessels and nerves become irritated, causing intense pain and sensitivity. Moreover, as the infection progresses, it can spread beyond the pulp chamber into the root canals, resulting in further tissue damage and potential bone loss. This advanced stage of infection can lead to the formation of a dental abscess, characterized by severe pain, swelling, and discomfort.
To prevent these complications and preserve the tooth, a root canal treatment is often necessary. The procedure involves removing the infected or damaged pulp, thoroughly cleaning and shaping the root canals, and filling them with a biocompatible material to seal them off. This eliminates the source of infection, alleviates pain, and prevents further damage to the tooth and surrounding tissues.
Swelling
Swelling in the gums around a tooth can be a sign of an infection or inflammation that requires a root canal. This swelling is caused by the body’s response to the bacteria that have invaded the pulp of the tooth. The bacteria produce toxins that irritate the tissues around the tooth, causing them to swell.
- Pain: The swelling can put pressure on the nerves in the tooth, causing pain.
- Sensitivity: The swelling can also make the tooth more sensitive to hot and cold temperatures.
- Difficulty eating: The swelling can make it difficult to eat and chew.
- Pus: In some cases, the swelling can cause pus to drain from the tooth.
If you are experiencing any of these symptoms, it is important to see a dentist right away. A root canal may be necessary to save the tooth and prevent the infection from spreading.
Sensitivity
Increased sensitivity to hot or cold temperatures is a common symptom of a damaged or infected tooth. This sensitivity occurs because the dentin, the layer of the tooth beneath the enamel, has been exposed. Dentin contains tiny tubules that lead to the pulp of the tooth. When these tubules are exposed, they can transmit sensations of heat and cold directly to the pulp, causing pain.
There are several reasons why the dentin may become exposed, including:
- Tooth decay: Tooth decay can damage the enamel and dentin, exposing the tubules.
- Gum disease: Gum disease can damage the gums and bone that support the teeth, exposing the roots of the teeth. The roots of the teeth are covered in dentin, so when they are exposed, the tubules can become exposed as well.
- Cracked or chipped teeth: Cracked or chipped teeth can also expose the dentin.
If you are experiencing increased sensitivity to hot or cold temperatures, it is important to see a dentist right away. This sensitivity could be a sign of a more serious problem, such as a cavity or an infected tooth. A root canal may be necessary to save the tooth and prevent further damage.
Here is a table summarizing the key points about sensitivity and the need for a root canal:
| Symptom | Cause | Treatment |
|---|---|---|
| Increased sensitivity to hot or cold temperatures | Damage to the dentin | Root canal |
Understanding the connection between sensitivity and the need for a root canal can help you to make informed decisions about your oral health. If you are experiencing increased sensitivity to hot or cold temperatures, be sure to see a dentist right away.
Discoloration
Discoloration of a tooth, presenting as a darkened or discolored appearance, often indicates underlying damage to the pulp, the innermost part of the tooth that contains nerves and blood vessels. Understanding this connection is crucial in determining the necessity of a root canal procedure.
- Pulp Damage: Pulp damage can occur due to various factors, including deep decay, trauma, or a cracked tooth. When the pulp becomes compromised, it can lead to inflammation and infection, affecting the tooth’s vitality and causing discoloration.
- Bacterial Invasion: Bacterial invasion into the pulp can result in the production of waste products and toxins that discolor the tooth. These bacteria thrive in the nutrient-rich environment of the pulp, causing further damage and discoloration over time.
- Hemorrhage: Trauma or injury to the tooth can lead to bleeding within the pulp chamber. The breakdown of red blood cells releases hemoglobin, which can seep into the dentin, causing a pinkish or brownish discoloration of the tooth.
- Dentin Changes: In some cases, age-related changes or certain medications can affect the dentin, the layer of the tooth beneath the enamel. These changes can lead to increased porosity and discoloration of the tooth.
Discoloration of a tooth, particularly when accompanied by other symptoms such as pain, sensitivity, or swelling, warrants prompt dental evaluation. A root canal may be necessary to address the underlying pulp damage, remove the infection, and restore the health and appearance of the tooth.
Abscess
The formation of an abscess at the root of a tooth is a severe dental condition that underscores the necessity of root canals. An abscess develops when a bacterial infection, often originating from untreated tooth decay or gum disease, spreads to the deepest part of the tooth, the pulp. This infection can cause significant pain, swelling, and discomfort, potentially leading to further complications if left untreated.
Suggested read: Uncover Hidden Truths: Symptoms of an Impending Root Canal Unveiled
The presence of an abscess is a clear indication that a root canal is necessary to address the underlying infection and prevent further damage. During a root canal procedure, the infected pulp is removed, the root canals are cleaned and disinfected, and the tooth is sealed to prevent re-infection. This treatment aims to eliminate the infection, alleviate pain, and preserve the tooth’s structure.
Understanding the connection between an abscess and the need for a root canal is crucial for maintaining good oral health. If you experience persistent tooth pain, sensitivity, or swelling, it is essential to seek prompt dental attention. Early diagnosis and treatment can prevent the formation of an abscess and the need for more extensive dental interventions.
| Abscess Formation | Root Canal |
|---|---|
| Cause: Untreated tooth decay or gum disease | Purpose: Remove infected pulp, clean and disinfect root canals |
| Symptoms: Pain, swelling, discomfort | Outcome: Elimination of infection, pain relief, preservation of tooth |
| Consequences: Further complications if left untreated | Importance: Prevents abscess formation and related complications |
Jaw pain
Understanding this connection is crucial for comprehensive dental care. Jaw pain, often a symptom of an underlying dental issue, can be effectively addressed through root canal treatment in specific scenarios. A root canal becomes necessary when an infection or inflammation affects the pulp, the innermost part of the tooth containing nerves and blood vessels. When the infection spreads to the root of the tooth, it can cause significant discomfort and pain that may radiate to the jaw.
The pain experienced in the jaw is a result of the body’s response to the infection. The inflammation and swelling associated with the infected tooth can put pressure on the surrounding nerves and tissues, leading to jaw pain. In such cases, a root canal offers a solution by removing the infected pulp, cleaning and disinfecting the root canals, and sealing the tooth to prevent further infection. By eliminating the source of the infection, a root canal can effectively alleviate jaw pain and restore oral health.
Recognizing the connection between jaw pain and the need for a root canal empowers individuals to make informed decisions about their dental care. Experiencing persistent or severe jaw pain alongside other symptoms such as tooth pain, sensitivity, or swelling warrants prompt dental attention. A timely diagnosis and appropriate treatment, including a root canal if necessary, can prevent the spread of infection, preserve the tooth, and alleviate jaw pain, promoting overall oral well-being.
FAQs on “Why Do I Need a Root Canal?”
Understanding the necessity of a root canal is crucial for maintaining good oral health. Here are some frequently asked questions that provide further insights into this dental procedure:
Question 1: What are the signs that I may need a root canal?
Persistent toothache, sensitivity to hot or cold, swelling or tenderness in the gums, and discoloration of the tooth are all potential indicators of the need for a root canal.
Question 2: Why is a root canal necessary if I have a toothache?
A toothache often signals an infection in the pulp, the innermost part of the tooth. If left untreated, the infection can spread to the surrounding tissues and cause severe pain and complications.
Question 3: Can a root canal save my tooth?
Yes, a root canal aims to preserve the tooth by removing the infected or damaged pulp and sealing the root canals to prevent further infection. It can effectively alleviate pain and restore the tooth’s functionality.
Question 4: Is a root canal painful?
During the procedure, local anesthesia is used to numb the area, minimizing any discomfort. After the root canal, some mild pain or sensitivity may occur, which can be managed with over-the-counter pain relievers.
Question 5: What happens if I don’t get a root canal when I need one?
Neglecting a necessary root canal can lead to severe pain, the spread of infection, and ultimately the loss of the tooth. It can also affect overall health by causing infections in other parts of the body.
Question 6: How can I prevent the need for a root canal?
Regular dental checkups, good oral hygiene practices, and promptly addressing any signs of tooth decay or gum disease can help prevent the development of conditions that may require a root canal.
Suggested read: Uncover the Hidden Signs: Your Ultimate Guide to Oil Change Necessity
Understanding these FAQs empowers you to make informed decisions about your dental health. If you have any concerns or experience symptoms that may indicate the need for a root canal, don’t hesitate to consult with a qualified dentist for proper diagnosis and treatment.
Transition to the next article section: Importance of Regular Dental Checkups for Maintaining Oral Health
Tips on Why You May Need a Root Canal
Understanding the reasons behind needing a root canal is crucial for maintaining good oral health. Here are some tips to help you identify the signs and symptoms that may indicate the necessity of a root canal:
Tip 1: Persistent Toothache
A persistent toothache that doesn’t subside with over-the-counter pain relievers may be a sign of an infected or inflamed pulp. Seeking prompt dental attention is essential to prevent further complications.
Tip 2: Sensitivity to Hot or Cold
Experiencing sharp pain or discomfort when consuming hot or cold beverages or foods could indicate damage to the tooth’s nerve. This sensitivity often signals the need for a root canal to address the underlying issue.
Tip 3: Swelling or Tenderness in the Gums
Inflammation or swelling in the gums around a specific tooth can be a symptom of an infection that has spread to the root of the tooth. Ignoring this sign can lead to more severe pain and complications.
Tip 4: Discoloration of the Tooth
A tooth that has darkened or changed color may indicate pulp damage or infection. This discoloration often occurs when the nerve or blood supply to the tooth has been compromised.
Tip 5: Jaw Pain
In some cases, an infected tooth can cause pain that radiates to the jaw. This pain is often a result of the infection spreading to the surrounding tissues and nerves.
Summary:
Being aware of the signs and symptoms that may indicate the need for a root canal is essential for maintaining good oral health. If you experience any of these issues, it is crucial to schedule an appointment with your dentist for proper diagnosis and treatment. Ignoring the need for a root canal can lead to severe pain, further complications, and even tooth loss.
Transition to the article’s conclusion:
Understanding the reasons why you may need a root canal empowers you to make informed decisions about your oral health. By recognizing the symptoms and seeking timely treatment, you can preserve your teeth, prevent pain, and maintain a healthy smile.
Suggested read: Discover the Profound Truths of "People Need the Lord"
Conclusion
Understanding the reasons behind needing a root canal is crucial for maintaining good oral health. This article has explored the various signs and symptoms that may indicate the necessity of a root canal, including persistent toothaches, sensitivity to hot or cold, swelling or tenderness in the gums, discoloration of the tooth, and even jaw pain. Recognizing these indicators and seeking timely treatment can prevent severe pain, further complications, and tooth loss.
A root canal is a dental procedure that aims to preserve a damaged or infected tooth by removing the affected pulp and sealing the root canals. It is a safe and effective treatment that can alleviate pain, restore functionality, and maintain a healthy smile. If you experience any of the symptoms discussed above, it is highly recommended to schedule an appointment with a qualified dentist for proper diagnosis and treatment.
Youtube Video: