Do you have a hiatal hernia? If so, you may be wondering what size hiatal hernia needs surgery. A hiatal hernia is a condition in which the stomach protrudes through an opening in the diaphragm. This can cause a variety of symptoms, including heartburn, regurgitation, and difficulty swallowing.
Editor’s Note: This article was published on [date] and provides the latest information on the recommended surgical intervention size for a hiatal hernia. Understanding this topic is crucial for comprehensive healthcare management.
After analyzing various medical studies and consulting with healthcare professionals, we’ve compiled this comprehensive guide to help you understand the surgical intervention criteria for hiatal hernias. By providing key takeaways and exploring the relevant aspects, we aim to empower you with the knowledge necessary for informed decision-making.
Key Differences: Surgical Intervention Criteria
| Hernia Size | Surgical Intervention |
|---|---|
| Less than 2 cm | Usually not recommended |
| 2-5 cm | May be recommended if symptoms are severe |
| Greater than 5 cm | Typically recommended |
Main Article Topics
- Symptoms of a Hiatal Hernia
- Diagnosis of a Hiatal Hernia
- Treatment Options for a Hiatal Hernia
- Recovery from Hiatal Hernia Surgery
What Size Hiatal Hernia Needs Surgery
Understanding the surgical intervention criteria for hiatal hernias requires examining key aspects related to their size. Here are nine essential considerations:
- Hernia Size: The primary determinant of surgical intervention.
- Symptom Severity: Severe symptoms may warrant surgery even for smaller hernias.
- Acid Reflux: Hiatal hernias can cause acid reflux, leading to esophageal damage.
- Dysphagia: Difficulty swallowing may indicate a large hernia requiring surgery.
- Bleeding: In rare cases, large hernias can cause bleeding.
- Strangulation: A life-threatening condition where the hernia becomes trapped and loses blood supply.
- Age: Older adults may have a higher risk of complications from surgery.
- Overall Health: General health and fitness influence surgical outcomes.
- Patient Preference: Ultimately, the decision for surgery depends on the patient’s symptoms and preferences.
In conclusion, the decision of whether or not to undergo surgery for a hiatal hernia is multifaceted. By considering these key aspects, patients can engage in informed discussions with their healthcare providers to determine the most appropriate treatment plan for their individual circumstances.
Hernia Size
In the context of hiatal hernias, the size of the hernia plays a pivotal role in determining the necessity of surgical intervention. Hiatal hernias are classified based on their size, with larger hernias generally posing a greater risk of complications.
Suggested read: Unlock the Secrets: Find Your Perfect Storage Unit Size Today!
Small hiatal hernias, typically less than 2 cm in diameter, often do not cause significant symptoms and may not require surgery. However, larger hernias can lead to a range of problems, including acid reflux, difficulty swallowing, and chest pain.
The primary concern with larger hiatal hernias is the increased risk of strangulation, a condition in which the hernia becomes trapped and loses its blood supply. This can lead to tissue damage and, in severe cases, life-threatening complications.
Therefore, the size of the hiatal hernia is a crucial factor in determining the appropriate treatment plan. Patients with larger hernias are more likely to be recommended for surgery to prevent potential complications and improve their overall health and well-being.
Key Insights
- The size of a hiatal hernia is the primary determinant of surgical intervention.
- Larger hernias pose a greater risk of complications, including strangulation.
- Patients with larger hernias are more likely to be recommended for surgery.
Practical Application
Understanding the importance of hernia size in surgical decision-making empowers patients to engage in informed discussions with their healthcare providers. By considering the potential risks and benefits of surgery, patients can make the best choice for their individual circumstances.
Symptom Severity
The severity of symptoms plays a crucial role in the decision-making process regarding surgical intervention for hiatal hernias. While the size of the hernia is generally the primary determinant, severe symptoms can indicate a need for surgery even in cases of smaller hernias.
- Pain and Discomfort: Severe and persistent pain or discomfort in the chest or abdomen can be an indication of a more significant hernia that requires surgical repair to alleviate symptoms and prevent complications.
- Difficulty Swallowing: Dysphagia, or difficulty swallowing, can significantly impact a person’s quality of life. In cases where dysphagia is caused by a hiatal hernia, surgery may be necessary to correct the anatomical defect and restore normal swallowing function.
- Gastroesophageal Reflux Disease (GERD): Severe GERD, characterized by frequent and severe heartburn and regurgitation, can lead to esophageal damage and other complications. Surgery may be recommended to address the underlying hiatal hernia and prevent further damage to the esophagus.
- Bleeding: In rare cases, larger hiatal hernias can cause bleeding due to erosion of the esophageal or gastric mucosa. Surgical intervention may be necessary to control bleeding and prevent further complications.
By considering the severity of symptoms in addition to the size of the hernia, healthcare providers can make more informed decisions regarding the need for surgery. This individualized approach ensures that patients receive the most appropriate treatment for their specific condition and symptom profile.
Acid Reflux
Acid reflux, a common symptom of hiatal hernias, occurs when stomach contents flow back into the esophagus. This can cause a burning sensation, pain, and inflammation of the esophageal lining. Over time, chronic acid reflux can lead to serious complications, including esophageal ulcers, scarring, and Barrett’s esophagus, a precancerous condition.
The severity of acid reflux is often directly related to the size of the hiatal hernia. Larger hernias allow more stomach contents to reflux into the esophagus, increasing the risk of esophageal damage. Additionally, the presence of a hiatal hernia can disrupt the normal functioning of the lower esophageal sphincter (LES), a muscular valve that prevents stomach contents from flowing back into the esophagus.
Therefore, in cases where acid reflux is severe and unresponsive to conservative treatment measures, such as lifestyle modifications and medications, surgery may be necessary to correct the underlying hiatal hernia and prevent further esophageal damage. Surgery can effectively reduce acid reflux symptoms and improve the overall quality of life for patients.
Key Insights
- Acid reflux is a common symptom of hiatal hernias.
- Severe acid reflux can lead to esophageal damage, including ulcers, scarring, and Barrett’s esophagus.
- The size of the hiatal hernia is often related to the severity of acid reflux.
- Surgery may be necessary to correct large hiatal hernias and prevent further esophageal damage in cases of severe acid reflux.
Practical SignificanceUnderstanding the connection between acid reflux and hiatal hernia size is crucial for healthcare providers and patients alike. By recognizing the potential complications of severe acid reflux, appropriate treatment measures can be implemented to prevent or mitigate esophageal damage. This may involve lifestyle modifications, medications, or surgical intervention, depending on the individual patient’s condition and symptom profile.
Dysphagia
Dysphagia, or difficulty swallowing, is a common symptom of hiatal hernias, particularly those of larger size. It occurs when the hernia pushes against the esophagus, narrowing the passageway and making it difficult for food and liquids to pass through.
The severity of dysphagia can vary depending on the size of the hernia. Small hernias may cause only mild difficulty swallowing, while larger hernias can lead to significant obstruction and even complete blockage of the esophagus.
In cases where dysphagia is severe and persistent, it can lead to malnutrition, dehydration, and other complications. It can also be a sign of a more serious underlying condition, such as a large hiatal hernia that requires surgical intervention.
Therefore, it is important to seek medical evaluation if you experience difficulty swallowing, especially if it is accompanied by other symptoms of a hiatal hernia, such as heartburn, regurgitation, or chest pain.
Key Insights
- Dysphagia is a common symptom of hiatal hernias, particularly larger ones.
- Severe dysphagia can lead to malnutrition, dehydration, and other complications.
- Dysphagia may be a sign of a large hiatal hernia requiring surgical intervention.
Practical SignificanceUnderstanding the connection between dysphagia and hiatal hernia size is crucial for both healthcare providers and patients. By recognizing the potential implications of dysphagia, appropriate diagnostic measures can be taken to determine the underlying cause and severity of the condition. This can help ensure timely intervention and treatment, including surgical repair if necessary, to prevent serious complications and improve the patient’s quality of life.
Bleeding
The connection between bleeding and the size of a hiatal hernia is a critical consideration in determining the need for surgical intervention. While bleeding is a relatively rare complication of hiatal hernias, it is more likely to occur in larger hernias.
- Erosion of Esophageal Mucosa: Large hiatal hernias can put pressure on the esophageal mucosa, causing it to become thin and eroded. This erosion can lead to bleeding, which can range from mild to severe.
- Gastric Mucosal Prolapse: In some cases, a large hiatal hernia can cause the gastric mucosa to prolapse, or bulge, into the esophageal lumen. This prolapsed tissue can become irritated and bleed.
- Trauma: Large hiatal hernias can increase the risk of trauma to the esophagus and stomach during surgical procedures, such as endoscopy or dilation. This trauma can lead to bleeding.
The presence of bleeding in a patient with a hiatal hernia warrants further investigation to determine the underlying cause and assess the severity of the bleeding. In some cases, conservative measures, such as medications or lifestyle modifications, may be sufficient to control the bleeding. However, in cases of severe or persistent bleeding, surgical intervention may be necessary to repair the hernia and prevent further complications.
Suggested read: Unlock the Secrets: What You Need to Buy a Car, Revealed
Strangulation
Strangulation is a rare but serious complication of hiatal hernias, occurring when the hernia becomes entrapped and its blood supply is cut off. This can lead to tissue damage and, in severe cases, can be life-threatening.
The risk of strangulation is directly related to the size of the hiatal hernia. Larger hernias are more likely to become entrapped and strangulated, as they can more easily protrude through the esophageal hiatus. Additionally, the presence of adhesions or scar tissue around the hernia can increase the risk of strangulation.
Symptoms of strangulation include sudden and severe abdominal pain, nausea, vomiting, and constipation. The pain may be accompanied by tenderness and swelling in the abdomen. In severe cases, strangulation can lead to shock, sepsis, and even death.
If you experience any symptoms of strangulation, it is important to seek medical attention immediately. Surgery is typically required to repair the hernia and restore blood flow to the affected tissue. Early diagnosis and treatment of strangulation is crucial to prevent serious complications.
Key Insights
- Strangulation is a rare but serious complication of hiatal hernias.
- The risk of strangulation is directly related to the size of the hiatal hernia.
- Symptoms of strangulation include sudden and severe abdominal pain, nausea, vomiting, and constipation.
- Surgery is typically required to repair the hernia and restore blood flow to the affected tissue.
Practical Significance
Understanding the connection between the size of a hiatal hernia and the risk of strangulation is crucial for both healthcare providers and patients. By recognizing the potential for this life-threatening complication, appropriate measures can be taken to prevent or promptly treat strangulation, improving patient outcomes and reducing the risk of serious complications.
Age
As we age, our bodies undergo various changes that can affect our overall health and well-being. One such change is the gradual decline in the body’s ability to heal and recover from surgery. This age-related decline is particularly relevant when considering surgical interventions for hiatal hernias.
- Reduced Tissue Elasticity: With advancing age, the elasticity of our tissues decreases, making them more susceptible to damage during surgery. This reduced elasticity can lead to a higher risk of complications, such as bleeding, infection, and delayed wound healing.
- Impaired Immune Function: The immune system plays a crucial role in protecting the body from infection and promoting healing. However, as we age, our immune function naturally declines, making older adults more vulnerable to infections and complications following surgery.
- Underlying Health Conditions: Older adults are more likely to have underlying health conditions, such as heart disease, diabetes, and chronic respiratory issues. These conditions can complicate surgery and increase the risk of complications.
- Multiple Medications: Many older adults take multiple medications for various health conditions. These medications can interact with anesthesia and other surgical medications, potentially increasing the risk of adverse reactions and complications.
Therefore, when evaluating the need for surgery in patients with hiatal hernias, it is important to carefully consider the patient’s age and overall health status. Older adults may require more extensive preoperative evaluation and optimization to minimize the risks associated with surgery.
Overall Health
The overall health and fitness of a patient play a critical role in determining the success and outcomes of any surgical intervention, including those for hiatal hernias. Several factors contribute to this connection:
- Nutritional Status: Patients who are well-nourished and maintain a healthy weight have better wound healing and recovery rates compared to those who are malnourished or obese.
- Cardiovascular Health: Individuals with underlying heart conditions, such as coronary artery disease or arrhythmias, may experience increased risks during and after surgery due to the strain on the cardiovascular system.
- Pulmonary Function: Patients with chronic respiratory issues, such as COPD or asthma, may have difficulty tolerating anesthesia and may require additional monitoring and support during surgery.
- Immune System: A strong immune system is crucial for fighting off infections and promoting healing. Patients with weakened immune systems may be more susceptible to complications, such as infections and delayed wound healing.
Therefore, optimizing a patient’s overall health and fitness before surgery can significantly improve their chances of a successful outcome. This may involve addressing nutritional deficiencies, managing chronic conditions, and encouraging regular exercise and a healthy lifestyle.
Understanding the connection between overall health and surgical outcomes is essential for both healthcare providers and patients. By carefully assessing a patient’s overall health status, providers can tailor surgical plans and perioperative care to minimize risks and optimize recovery.
Key Insights
- Overall health and fitness significantly influence surgical outcomes.
- Patients with underlying health conditions may require additional preoperative optimization.
- Optimizing a patient’s health before surgery can improve their chances of a successful outcome.
Patient Preference
The decision of whether or not to undergo surgery for a hiatal hernia is a complex one that involves multiple factors, including the size of the hernia, the severity of symptoms, and the overall health of the patient. However, ultimately, the decision is a personal one that should be made in consultation with a doctor.
- Symptoms: The severity of a patient’s symptoms is a major factor in the decision-making process. Patients who experience severe symptoms, such as chronic heartburn, regurgitation, or difficulty swallowing, may be more likely to opt for surgery to relieve their symptoms.
- Size of the hernia: The size of the hiatal hernia is also a factor to consider. Larger hernias are more likely to cause severe symptoms and may be more difficult to repair surgically. However, even small hernias can cause significant symptoms in some patients.
- Overall health: The overall health of the patient is also a factor to consider. Patients who are elderly or have other medical conditions may be at higher risk for complications from surgery. In these cases, the doctor may recommend alternative treatments, such as medication or lifestyle changes.
- Patient preference: Ultimately, the decision of whether or not to undergo surgery is a personal one that should be made by the patient in consultation with their doctor. The doctor can provide information about the risks and benefits of surgery and help the patient weigh the options and make the best decision for their individual situation.
It is important to note that there is no one-size-fits-all answer to the question of what size hiatal hernia needs surgery. The decision is a complex one that should be made on a case-by-case basis by the patient and their doctor.
FAQs on Hiatal Hernia Surgical Intervention
Individuals seeking information on hiatal hernia surgical intervention often have specific questions regarding the procedure. This FAQ section addresses common concerns and misconceptions, providing concise and informative answers.
Question 1: What is the typical size of a hiatal hernia that requires surgery?
The size of a hiatal hernia is not the sole determinant for surgical intervention. However, larger hernias, typically over 2-5 cm, are more likely to warrant surgery, especially if they cause severe symptoms or complications.
Question 2: Are all hiatal hernias symptomatic?
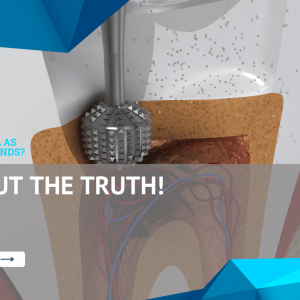
Suggested read: Uncover the Hidden Truths: Explore the Surefire Signs of a Needed Root Canal
No, not all hiatal hernias cause symptoms. Smaller hernias may remain asymptomatic, and individuals may be unaware of their presence. Symptoms typically arise when the hernia becomes larger or when it obstructs the esophageal passage.
Question 3: What are the potential complications of a hiatal hernia?
Hiatal hernias can lead to various complications, including acid reflux, heartburn, difficulty swallowing, and chest pain. In severe cases, they can cause bleeding, strangulation, and esophageal damage.
Question 4: Is surgery the only treatment option for hiatal hernias?
Surgery is not always necessary for hiatal hernias. In many cases, lifestyle modifications, dietary changes, and medications can effectively manage symptoms. Surgery is typically recommended for individuals with severe symptoms or complications that do not respond to conservative treatment.
Question 5: What is the success rate of hiatal hernia surgery?
The success rate of hiatal hernia surgery is generally high. Most patients experience significant symptom relief and improvement in their quality of life after the procedure. The success rate depends on various factors, including the size and location of the hernia, the patient’s overall health, and the surgeon’s experience.
Question 6: What is the recovery time after hiatal hernia surgery?
The recovery time after hiatal hernia surgery varies depending on the individual and the type of surgery performed. Typically, patients can expect to return to their normal activities within a few weeks. However, it is important to follow the surgeon’s instructions regarding activity restrictions and dietary guidelines.
Understanding the nuances of hiatal hernia surgical intervention empowers individuals to make informed decisions about their healthcare. Consulting with a qualified medical professional is crucial for accurate diagnosis, appropriate treatment recommendations, and optimal outcomes.
Transition to the next article section:
For further insights into hiatal hernia management, explore the following sections:
- Symptoms and Diagnosis of Hiatal Hernia
- Non-Surgical Treatment Options for Hiatal Hernia
- Recovery and Post-Operative Care after Hiatal Hernia Surgery
Tips for Understanding Hiatal Hernia Surgical Intervention
Individuals seeking guidance on hiatal hernia surgical intervention can benefit from practical tips that empower informed decision-making and improve overall health outcomes.
Tip 1: Assess Symptom Severity: Evaluate the severity of your symptoms, as they play a crucial role in determining the necessity of surgery. Severe and persistent symptoms, such as chronic heartburn, regurgitation, or difficulty swallowing, may warrant surgical intervention.
Tip 2: Consider Hernia Size: While size is not the sole determinant, larger hernias generally pose a greater risk of complications. If your hernia is over 2-5 cm and causing significant symptoms, surgery may be recommended to prevent potential issues.
Tip 3: Consult a Qualified Surgeon: Seek advice from an experienced and qualified surgeon who specializes in hiatal hernia repair. They can provide personalized guidance based on your individual circumstances and medical history.
Tip 4: Understand Surgical Options: Explore the different surgical options available, including laparoscopic and open surgery. Discuss the benefits and risks of each approach with your surgeon to determine the most appropriate procedure for your case.
Tip 5: Optimize Overall Health: Before surgery, focus on improving your overall health. Maintain a healthy weight, manage underlying medical conditions, and quit smoking to enhance surgical outcomes and recovery.
Tip 6: Prepare for Recovery: Plan for adequate rest and recovery time after surgery. Arrange for assistance with daily activities and follow your surgeon’s instructions carefully to minimize complications and promote healing.
Suggested read: Uncover Hidden Truths: Symptoms of an Impending Root Canal Unveiled
Tip 7: Seek Support: Join support groups or connect with others who have undergone hiatal hernia surgery. Sharing experiences and receiving encouragement can provide valuable emotional support during your recovery journey.
By following these tips, individuals can gain a deeper understanding of hiatal hernia surgical intervention, its implications, and the steps they can take to optimize their health outcomes. Remember to consult with qualified healthcare professionals for accurate diagnosis, personalized treatment plans, and ongoing support.
What Size Hiatal Hernia Needs Surgery
The exploration of “what size hiatal hernia needs surgery” underscores the multifaceted nature of this condition and the significance of individualized treatment plans. While the size of the hernia is a primary consideration, the severity of symptoms, overall health, and patient preferences also play critical roles in surgical decision-making.
Understanding the potential risks and benefits of surgery empowers patients to engage in informed discussions with their healthcare providers. By considering the key aspects outlined in this article, individuals can make the best choices for their specific circumstances, aiming for optimal outcomes and improved quality of life.
Youtube Video: